Hysterectomy is the surgical removal of the uterus. The reasons for performing this surgery include abnormal bleeding, uterine prolapse, fibroids, and cancer.
After the removal of the uterus, only two things change: you will no longer have menstrual periods, and you will not be able to get pregnant. Unless your ovaries are removed, you will not enter menopause, and hormonally, sexually, and emotionally, nothing else will change for you.
Recovery typically takes four to six weeks, depending on the type of surgery you have.
For more information about hysterectomy, you can contact us and schedule an appointment.
Basic Information about Hysterectomy
- The uterus is the place where the baby grows during pregnancy.
- Hysterectomy is the surgical removal of the uterus and likely the cervix.
- Depending on the reason for the surgery, a hysterectomy may include the removal of surrounding organs and tissues, such as the fallopian tubes and ovaries.
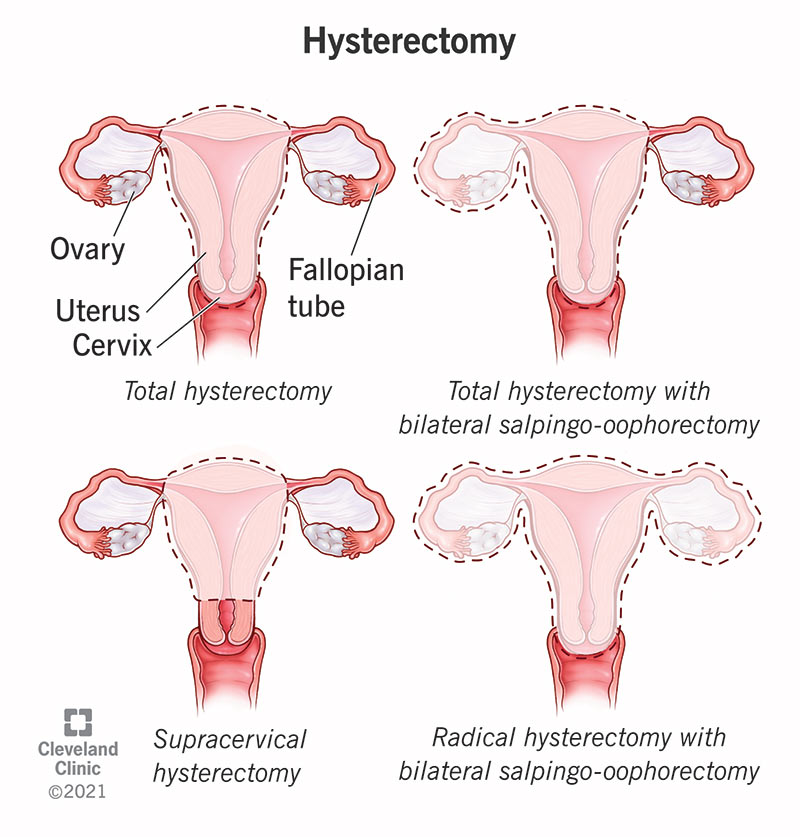
What Are the Different Types of Hysterectomy?
Your doctor will guide you on the type of hysterectomy that is necessary based on your condition. This will determine whether your fallopian tubes and/or ovaries need to be removed.
- Total hysterectomy: Removal of the uterus and cervix, but leaving the ovaries.
- Supracervical hysterectomy: Only the upper part of the uterus is removed, leaving the cervix intact.
- Bilateral salpingo-oophorectomy with total hysterectomy: Removal of the uterus, cervix, fallopian tubes (salpingectomy), and ovaries (oophorectomy). If you have not gone through menopause, removal of the ovaries will trigger menopause symptoms.
- Salpingo-oophorectomy with radical hysterectomy: Removal of the uterus, cervix, fallopian tubes, ovaries, upper part of the vagina, and some surrounding tissues and lymph nodes. This type of hysterectomy is performed when cancer is present.
Why Is Hysterectomy Performed?
- Abnormal or heavy vaginal bleeding that cannot be controlled with other treatments.
- Severe pain associated with menstrual bleeding that cannot be controlled with other treatments.
- Leiomyomas or uterine fibroids (non-cancerous tumors).
- Increased pelvic pain that cannot be controlled with other treatments.
- Uterine prolapse (a weakened pelvic floor causing the uterus to “drop” into the vaginal canal), which can lead to urinary incontinence or difficulty with bowel movements.
- Cervical or uterine cancer or abnormalities that may lead to cancer.
- Conditions related to the uterine lining, such as hyperplasia, recurrent uterine polyps, or adenomyosis.
How Should I Prepare for a Hysterectomy?
Your doctor will explain the procedure in detail, including possible complications and side effects. If you have any concerns, make sure to consult your doctor.
What Happens During a Hysterectomy?
Your doctor will determine the best surgical method to perform the necessary hysterectomy based on your situation.
- First, an intravenous (IV) line will be placed in a vein in your arm to administer the necessary medications and fluids.
- During the procedure, you will be under general anesthesia, so you will not be awake; or you may receive regional anesthesia (epidural or spinal anesthesia), where medications are placed near the nerves in your back to block pain while you remain awake.
There are several different surgical approaches your healthcare provider may use to perform a hysterectomy:
Vaginal Hysterectomy:
- Your uterus is removed through an incision in the upper part of your vagina. No external incision is made.
- Resorbable stitches are placed inside the vagina.
- This is most commonly used for uterine prolapse and other benign (non-cancerous) conditions.
- It has the least complications and the fastest recovery time (up to four weeks) and is considered the preferred approach.
- Patients are often able to go home the same day of the surgery.
Laparoscopic Hysterectomy:
- A laparoscope (a thin tube with a video camera) is inserted into the lower abdomen through a small incision near the belly button.
- Surgical instruments are inserted through several other small incisions.
- Your uterus is removed in small pieces through the incisions in your abdomen or vagina.
- Some people go home the same day or after staying in the hospital for one night.
- Full recovery is shorter and less painful compared to abdominal hysterectomy.

Robot-Assisted Laparoscopic Hysterectomy:
- Your surgeon performs the procedure with the assistance of a robotic machine.
- A laparoscope is placed inside your abdomen to allow the pelvic area to be seen.
- Small, thin surgical instruments are inserted through three to five incisions around your belly button. The robotic arms and instruments are controlled by the surgeon.
- Recovery is similar to laparoscopic hysterectomy.
Abdominal Hysterectomy:
- Your uterus is removed through a cut about 10 cm long in your abdomen.
- The incision is either made from your belly button to your pubic bone or just above your genital hairline. The cuts are always cosmetically closed.
- This is most commonly used when cancer is involved, when the uterus is enlarged, or when the disease has spread to other pelvic areas.
- It usually requires a longer hospital stay (two days) and a longer recovery time.
How Long Does the Hysterectomy Procedure Take?
The procedure takes one to three hours. This time may vary depending on the size of the uterus, the need to open adhesions from previous surgeries, the need to remove scar tissue, and whether other tissues, such as endometrial tissue and other organs like your fallopian tubes or ovaries, need to be removed along with your uterus.
What Are the Most Common Side Effects of Hysterectomy?
Some of the most common side effects of hysterectomy include vaginal discharge (which may appear up to six weeks after surgery) and irritation at the incision sites.
If your ovaries were removed during the hysterectomy, you may experience menopause symptoms, including hot flashes, night sweats, and mood swings.
More serious complications include:
- Infection.
- Blood clots.
- Injury to other organs (rare).
Before having the surgery, talk to your doctor about what to expect during and after your hysterectomy. Ask them about recovery and any complications.
What Is Recovery Like After a Hysterectomy?
Your recovery will depend on the type of surgery and your individual health. Typically, recovery from a hysterectomy takes 4-6 weeks.
It is important to follow your doctor’s instructions during your recovery. After surgery, you will be instructed to avoid heavy lifting, avoid sexual activity, and avoid driving for several weeks. You should also avoid baths or swimming for several weeks to reduce the risk of infection.
What Are the Alternatives to Hysterectomy?
Your healthcare provider will work with you to develop the best treatment plan for your symptoms or condition. If a hysterectomy is not medically necessary, some alternatives that may be considered include:
- Watchful waiting to see if the condition improves or resolves on its own.
- Taking medications, such as birth control pills, to manage painful periods or abnormal bleeding.
- Cauterizing the inner lining of the uterus to control heavy bleeding.
- Procedures or surgery to remove uterine fibroids.
- Exercises for uterine prolapse that help strengthen the muscles in your uterus.
- Using a pessary to “support” the uterus if you have uterine prolapse.
- Surgery to treat endometriosis or vaginal bleeding that doesn’t require the removal of the entire uterus.
 EN
EN TR
TR
